Prescription Drug Coverage
Prescription drug coverage is automatically included with all of K-C's medical plan options.
The information below describes your prescription drug benefit if you participate in any Anthem medical plan option. CVS/caremark is the Pharmacy Benefit Manager (PBM) for these medical plans, meaning they handle all of the prescription benefits. If you’re enrolled in another medical plan, check with your insurance company for details about your prescription drug benefit.

Check the Types of Your Prescriptions
The chart below shows the different prescription types, how the CDHP plan options cover them, and the actions required. Log in to your account to see specific information for your plan. Remember, under the Anthem plan options you pay out of pocket until you reach your deductible. If you choose to use a brand name drug instead of its generic equivalent, you (or the member) will pay the difference between the generic price and the brand name price.
| Type | Description | Example | Cost | Action |
|---|---|---|---|---|
| Short-term | Medications taken for a limited amount of time with a limited amount of refills. | Includes antibiotics, and pain medicine post-surgery. | You pay 100% of the discounted cost until you meet your annual deductible. | You can fill these prescriptions at any pharmacy in the CVS/caremark retail network, which includes independent pharmacies and many other chain pharmacies such as Walgreens and Walmart. Find a participating pharmacy online. |
| Long-term Preventive |
Medications taken to prevent certain health conditions and to maintain health. Preventive care does not include drugs for treatment of an existing disease or condition. These are determined by the Affordable Care Act (ACA). | Includes birth control, immunizations, colonoscopy prep, and smoking cessation products. To learn which are included, call CVS/caremark or log in online. | You pay $0 for preventive prescriptions. | You can fill these prescriptions at any pharmacy in the CVS/caremark retail network, which includes independent pharmacies and many other chain pharmacies such as Walgreens and Walmart. Find a participating pharmacy on CVS/caremark's website. |
| Long-term Maintenance* |
Medications taken by those who have risk factors for a disease or to prevent the reoccurrence of a disease. These are determined by the IRS Maintenance Guidelines and are subject to change. | Prescriptions to treat conditions like high blood pressure, high cholesterol, asthma, or diabetes. To learn which are included, call CVS/caremark or log in online. |
You pay $0 for certain maintenance prescriptions.* | Under the Mandatory Mail/Maintenance Choice Drug program, you can fill your 30-day maintenance prescription up to three times at your local pharmacy in the CVS/caremark retail network, which includes independent pharmacies and many other chain pharmacies such as Walgreens and Walmart. After the third fill, you’ll need to switch to a 90-day supply and you must use a CVS Pharmacy or the CVS mail-order pharmacy program in order for the deductible or coinsurance to apply. Note: If you request the same 30-day maintenance prescription a fourth time and/or don't use your local CVS pharmacy or the CVS mail-order pharmacy program, you'll pay 100% of the discounted cost. |
| Long-term Other |
Medications taken on an on-going basis that are not recognized by the ACA or IRS Maintenance Guidelines. | Includes prescriptions to treat thyroid conditions or post-menopausal symptoms | You pay 100% of the discounted cost until you meet your annual deductible. | Use the Mandatory Mail/Maintenance Choice Drug program or use a participating pharmacy in the CVS/caremark retail network to have your prescriptions filled. This includes independent pharmacies and many other chain pharmacies such as Walgreens and Walmart. |
| Specialty | For specialty drugs, such as certain drugs used to treat rheumatoid arthritis and psoriasis, you must use the CVS/caremark Specialty Pharmacy program or a CVS retail pharmacy. If you prefer, you can have the specialty pharmacy ship your prescription to a CVS retail pharmacy to pick up. | |||
*All generic long-term maintenance drugs are covered by K-C and you pay $0. Brand-name maintenance drugs in certain classes, where a generic alternative is available, are subject to 20% coinsurance until you reach the out-of-pocket maximum. If your health care provider certifies you’re unable to take a generic, call CVS/caremark to discuss your options.
Paying for Prescription Needs
When it’s time to pay for a prescription (Rx), here’s what to expect when using CVS/caremark:
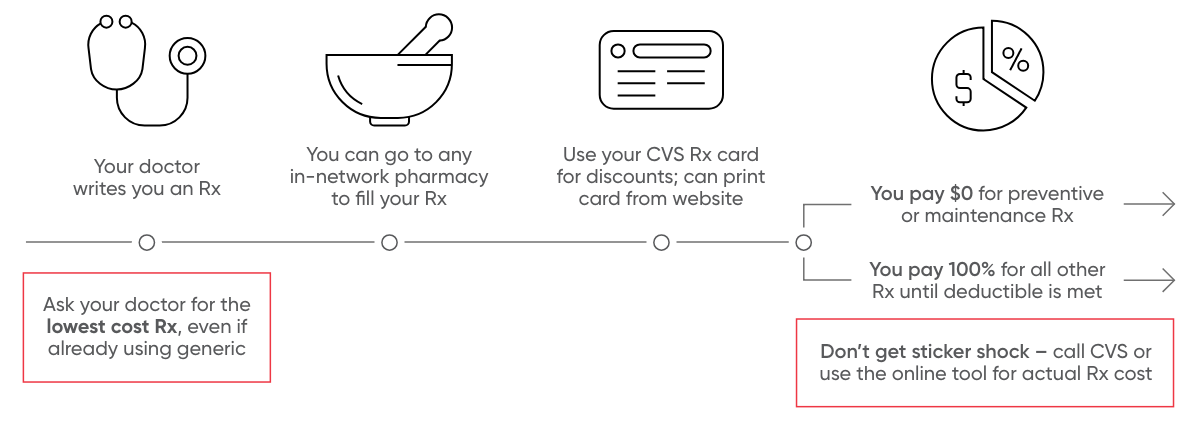
- Your doctor writes you a prescription. Use the CVS/caremark mobile app or website while at the doctor’s office to double check the coverage and cost for that prescription before you have it filled. Ask your doctor for the lowest cost prescription, even if you’re already using generic.
- You go to a local pharmacy to fill and pick up your prescription. Once you have a prescription from your doctor, use the CVS/caremark mobile app or website to find a local, in-network pharmacy to fill it at. Note that if it is a long-term prescription, you’ll be required to get on the CVS/caremark Mandatory Mail/Maintenance Choice Drug program after three fills at a local pharmacy.
- Use your CVS/caremark prescription card for discounts. Use your CVS/caremark prescription card to get the discounted cost and ensure those costs apply toward your annual deductible and out-of-pocket maximum. It also ensures that you get your eligible maintenance prescription for $0. If you don’t have your CVS/caremark prescription card, you can log into your CVS account and print a copy of it.
- You pay the pharmacy the amount owed. Use your Fidelity debit card or personal funds to pay the pharmacy what you owe. Remember, if it’s an eligible preventive or maintenance prescription, you’ll pay $0. For all other prescriptions, you’ll pay 100% of the discounted cost until you meet your annual deductible.
You have the option to fill your prescription outside of the CVS/caremark network (e.g. Amazon). If you can get your prescription filled for less elsewhere, you’re welcome to do so. You can even use your HSA dollars to pay for it. However, whatever you spend won’t run through the plan — meaning it won’t count toward your annual deductible or out-of-pocket maximum.
The Drug Formulary
CVS/caremark has a list of covered drugs called a formulary. The list includes both generic and preferred brand-name drugs. Non-preferred brand-name drugs may also be covered under the plan if medically necessary but are not listed on the formulary.
Things to remember when reviewing your drug list:
- Generics should always be your first choice when available and medically appropriate.
- Ask your doctor to consider prescribing a brand-name product from your preferred drug list if a generic is not available.
- This list is not all-inclusive and does not guarantee coverage by the plan.
Tools to Help
Don’t forget! Use the tools and resources available to you. Use the CVS/caremark website or mobile app to:
- Order and manage prescriptions
- Check your prescription coverage and benefits
- Manage costs and save money
- Access a printable CVS/caremark ID card
You can also call CVS/caremark and speak with a representative.
Need more help?
Caremark Customer Care
888-797-8911
Available 24/7, 365 days a year.





